Freedom from In-stent-Restenosis
Aug 17, 2022

New Delhi [India], August 17 (ANI/ATK): As India is celebrating 75 years of Independence with Azadi ka Mahotsav, The Field of Interventioncardiology since its inception by Adreas Gruntzig in 1977, can celebrate freedom from In-stent -restenosis (ISR)?
ISR can be considered the "Achilles heel" of modern Day Percutaneous Coronary interventions(PCI).
Restenosis: Restenosis is a gradual re-narrowing of the stented segment that occurs mostly between 3 to 12 months after stent placement. In-stent-restenosis rate has come down drastically with ISR rates of 30.1 per cent, 14.6 per cent, and 12.2 per cent for BMS, first-generation DES, and second-generation DES, respectively.ISR still occurs in approximately 3 to 10 per cent of patients within six to nine months.
Factors Associated With In-stent-restenosis(ISR)
We have learned that restenosis is a very complex process. With the advancement of technology, cardiac science is able to achieve a very low restenosis rate.
Imaging Technology-IVUS: Intravascular Ultrasound and OCT: optical Coherence Tomography
This Imaging technique helps in proper lesion characterization, vessel diameter assessment, and stent apposition which helps in the optimization of PCI which in long term translates into a low rate of ISR. Intracoronary imaging has a growing role in guiding and optimizing PCI, especially as PCI in more complex and high-risk subsets. Imaging should be used prior to, during, and after stent deployment to obtain maximum benefit from the use of imaging as it has an important role to play in all steps of a PCI procedure.
Stent Technology: Stentsgraduated from Bare metal stents, First Generation Drug-eluting stent(DES), Second generation DES, Ultrathin struts, and third generation DES, especially biodegradable polymers, polymer-free stents, and biodegradable stents on the basis of poly-L-lactide (PLLA) or magnesium. With the improvement in stent design and technology, there is a gradual decrease in the in-stent restenosis rate from 30 per cent to nearly 3 per cent with current-generation DES.
Polymer-free Stent: Currently in clinical usage are Polymer-free biolimus A9-eluting stents or with a biodegradable-polymer sirolimus-eluting stent or polymer-free sirolimus and probucol-eluting stents. In clinical trials, these polymer-free stents Showed noninferiority or numerically better outcomes than Stable polymer-based stents. Ten-year clinical outcomes of polymer-free versus durable polymer new-generation drug-eluting stent in patients with coronary artery disease with and without diabetes mellitus results of the Intracoronary Stenting and Angiographic Results: Test Efficacy of Sirolimus- and Probucol- and Zotarolimus-Eluting Stents (ISAR-TEST 5) trial shown comparable clinical outcomes.
Bioresorbable Stent: Bioresorbable scaffolds (BRS) represent the fourth evolution in myocardial revascularization therapies with extensive technological development and advancements. This stent is made of a metal that will automatically dissolve safely within the body two to three years after implantation and the patient's artery returns to its normal position. The primary metals in this category are magnesium-based and iron-based alloys, although recently zinc has also been investigated
Rotablation and Intravascular Lithotripsy (Shockwave Therapy)
For Calcified lesion rotablation was in place for a long time but the recent addition of user-friendly IVL provided more arsenals to the armamentarium of the Intervention cardiologist.
Shockwave intravascular lithotripsy (IVL) is a novel device used in patients with calcified blockages. Shockwave Medical Coronary IVL Catheter is a single-use disposable catheter that is connected to an integrated balloon and fitted with multiple lithotripsy machines. This machine creates a sonic pressure wave for the affected area. This sonic pressure wave breaks down calcium, creating space in the artery.
IVL popularity has been on the rise in view of a more user-friendly and short learning curve.
Plaque Modification-Cutting/Scoring Balloon and Open -NC- With the advent of these balloons fibrocalcific lesions can be dealt properly. This leads to proper vessel bed preparation which escalates into better clinical outcomes.
Cutting/Scoring Balloons
Cutting balloons are comprised of standard balloon catheters mounted with lateral metallic blades, which on inflation of the balloon incise into the treated stenotic plaque. Scoring balloons have a broadly similar mechanistic basis but employ low-profile nitinol wires (of the order of 125um) on the surface of the balloon catheter in a spiral formation.
OPEN -NC Balloon - OPN NC is a unique Swiss-made CE Marked Plaque Modification Device designed to perform in all complex lesions at Ultra-High Pressures. OPN NC utilizes Ultra-High Pressures to cause Calcium fracture or oppose Calcium to the arterial wall.OPN NC is designed with a dual layer technology to withstand Ultra-High Pressures which leads to uniform expansion even at pressures as high as 45 Bars.
Metabolic and Lifestyle Factors-Aggressive control of cholesterol, better management of diabetes, and healthy lifestyle measures are other factors that can prevent ISR. Lifestyle measures like non-smoking, keeping ideal body weight, daily physical activity, and a healthy balanced diet. Aim for good physical health and a stress-free mind.
Proper usage of these technologies in properly selected patients can lead to a very low rate of In-stent restenosis (ISR)and very low future clinical events. Achievement of near Zero ISR is a dream of every cardiologist and a requirement for every patient and with further developments in cardiac technology, that day is not very far. Believe my words, the conglomerate of lifestyle changes with proper Optimization of PCI can do wonders.
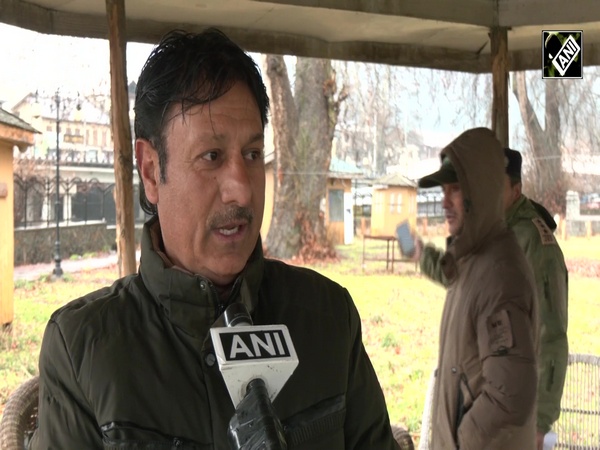
This article is written by Dr (Prof). Tarun Kumar, MD, DM, FSCAI, FACC, Professor Of Cardiology, ABVIMS &DR RML Hospital, New Delhi.
This story is provided by ATK. ANI will not be responsible in any way for the content of this article. (ANI/ATK)