National policy needed to destigmatise mental health: Experts on tackling suicides due to mental illness
Jun 15, 2020

By Joymala Bagchi
New Delhi [India], June 15 : With two separate incidents of alleged suicides reported in India yesterday, mental health and issues related are being discussed in volumes once again.
Actor Sushant Singh Rajput, aged 34, hung himself in his Mumbai residence on Sunday. In another incident yesterday in Delhi, a 56-year-old IRS officer allegedly consumed an acid-like substance in his car. A purported suicide note recovered from his car stated that official was unwell for some time and feared that he had infected his family of COVID-19, although his result came out negative.
According to the National Crime Record Bureau (NCRB), every year more than 1,00,000 people die due to suicide in India. There are various causes of suicides like professional/career problems, sense of isolation, abuse, violence, family problems, mental disorders, addiction to alcohol, financial loss, chronic pain etc.
As per NCRB's data for accidental deaths and suicides in India in 2018, a total of 1,34,516 suicides were reported in the country indicating an increase of 3.6 per cent in comparison to 2017 and the rate of suicides has increased by 0.3 per cent during 2018 over 2017.
Speaking with the medical fraternity, ANI attempted to explore the reasons behind the surge in suicide cases over the years in India.
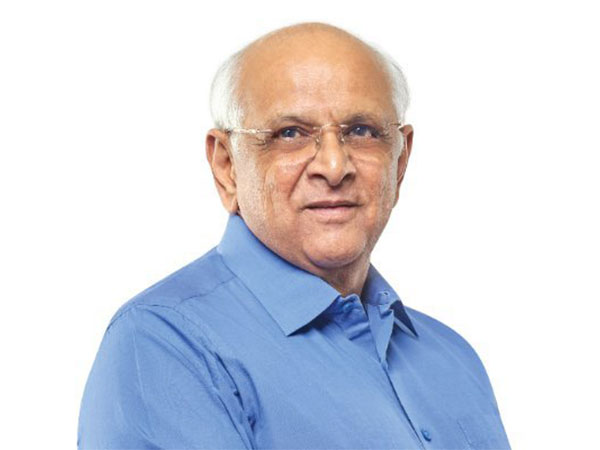
Dr Rajiv Mehta, Vice-Chairperson, Institute of Psychiatry and Behavioural Sciences, Sir Gangaram Hospital said, "As per data, India is a suicide capital where mental health needs to be addressed as a medical emergency. The shocking thing is that we lose young ones in such scenarios. The maximum number of suicide is happening in adolescence or early adulthood after which comes the old age population. We require a national helpline to prevent these things. We also require a great destigmatising programme of psychiatry. To tell the whole population of destigmatisation, we require a national policy."
As per data shared by Dr Mehta, 80 per cent of people in India who died of suicide, suffered from depression, is a medical and psychiatric illness that has biological components behind it.
Just like calcium deficiency leads to osteoporosis, thyroxin deficiency results in hypothyroidism, iron deficiency causes anaemia, serotonin deficiency reportedly leads to depression, as per mental health experts.
"Our body functions on chemicals. Emotions and behaviour are also run on chemicals, when they get depleted, depression happens. The reason for the depletion occurs from the demands in the brain which can be addressed as any kind of change, be it happy or negative," told Dr Mehta.
Doctors have reportedly demanded a National Suicide Prevention Programme from the Government of India (GoI), as present in most developed countries.
"The fear and the stress at this time of COVID-19 pandemic have exposed the vulnerabilities of all individuals. People with pre-existing mental health problems, poor coping skills, poor social support, substance use disorders like alcoholism and those with multiple life stressors have been grossly affected due to the uncertainty surrounding this pandemic," said Dr Manushree Gupta, Associate Professor, Department of Psychiatry VMMC (Vardhman Mahavir Medical College) and Safdarjung Hospital, Delhi.
Addressing the alleged suicide of Rajput, Dr Gupta said, "Every suicide is unfortunate and all efforts of the mental health professionals as well as the society should be driven to mitigate the risk of such tragedy. Mental health should not be forgotten after every such incidence rather mental health promotion should be a continuing drive in society."
"There is a lack of mental health professionals in smaller cities and semi-urban and rural areas of the country. The mental health gap in India is close to 80 per cent meaning that eight out of 10 people who require mental health care do not receive it due to various reasons," Dr Gupta added.
Mental health experts believe that the National Mental Health Programme and the Mental Healthcare Act, 2017 issued by the GoI has reduced stigmatisation remarkably.
Dr Nand Kumar, Professor of Psychiatry, All India Institute of Medical Sciences, Delhi said that as per a myth, people with stress develop depression, however, "the truth is depression can happen with or without stress".
"Educated people have definitely heard about depression but they are unaware. Being aware means comprehensive understanding. Once depression happens to me or my family, I have to be aware. Once treatment starts, the response varies between 30 per cent to 60 per cent which means 40 per cent may not respond faster and they need medications. However, most do not want to continue with the medication either because of stigma, or self-assessed side effects," Dr Kumar said.
Before COVID-19, 1.40 to 1.50 lakh suicides were reported every year, however, the National Crime Record Bureau will not keep a record of suicides because it is no more a criminal offence, Dr Kumar added.
Experts also suggest that importance of Psychological First Aid (PFA), an initiative issued by the World Health Organisation (WHO) in 2016, could be imparted as a public campaign to tackle the mental health crisis.