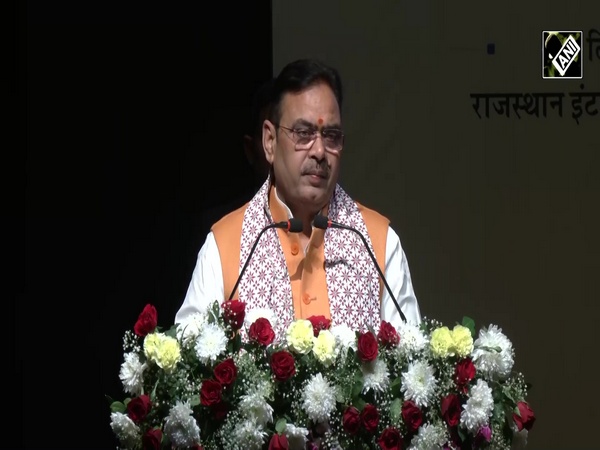
Study on over 1,600 patients suggests simple intervention to increase breast cancer cure rates: Director, Tata Memorial Centre
Sep 22, 2022

Mumbai (Maharashtra) [India], September 22 : A study on over 1,600 patients suggests a simple intervention to increase breast cancer cure and survival rates, said Dr Rajendra Badwe, Director Tata Memorial Centre (Tata Cancer Hospital) on Wednesday.
The landmark multi-centre Indian study on breast cancer gave good results, said Dr Badwe.
Out of the Sample size of 1,600 patients, 1,100 were from Tata Memorial Hospital itself and rest 500 patients were from 10 different centres from Kolhapur, Pune, Delhi, Bengaluru, Dr Badwe told ANI.
Earlier on September 12, Badwe presented the results of a landmark multi-centre Indian study on breast cancer at the European Society of Medical Oncology (ESMO) Congress in Paris that shows that simple, low-cost intervention significantly and substantially increases the cure rates and survival of breast cancer patients, with a benefit that is ongoing for several years after surgery.
"The trial in women undergoing breast cancer surgery involved the injection of a commonly used drug around the tumour, on the operating table, just prior to surgery The injection requires no additional expertise, is inexpensive, and can result in saving up to 100,000 lives annually globally. These benefits are substantial and were achieved with an intervention the cost of which was less than Rs 100 per patient," Badwe said.
Talking about the study, he further said, "For the comparison, benefits of far lesser magnitude have been achieved in early breast cancer patients by much more expensive, targeted drugs which cost more than ten lakhs per patient."
Dr Badwe said that the study took a decade from the idea being conceived and the study is completed.
While presenting the study at the conference, Dr Badwe had said, "This is the first study of its kind globally, that has shown a sizable benefit by single intervention prior to surgery. If implemented across the world, it has the capability to save over 100,000 lives annually. For scientists, it opens the window of peri-operative intervention to modulate the environment of cancer in such a way as to prevent its deleterious reaction to the act of surgery [observation]. Evolving low-cost interventions for cancer has been a mission of Tata Memorial Centre and Department of Atomic Energy for the benefit of Indian and global population and this study, supported by the Department of Atomic Energy, is a major step towards Atma Nirbhar Bharat."
The study, 'Effect of Peri-tumoral Infiltration of Local Anaesthetic Prior to Surgery on Survival in Early Breast Cancer is a randomized controlled trial, conceived and designed by Dr Badwe, who is the principal investigator. The study was conducted by investigators at 11 cancer centres in India including Tata Memorial Centre in Mumbai over an 11-year period between 2011 and 2022.
The study included 1,600 women with early breast cancer who were planned to be treated with surgery. Half of these patients, constituting the control group, received standard surgery followed by standard postoperative treatment including chemotherapy, hormone therapy and radiotherapy as per guidelines. The other half, constituting the intervention group, received an injection of a commonly used local anaesthesia agent, 0.5% lidocaine, all around the tumour, just prior to surgery. They then underwent standard surgery followed by the same postoperative treatment as was given in the control group.
Dr Badwe's previous research has suggested that there is a window of opportunity just prior to, during, and immediately after surgical removal of primary cancer when anti-cancer interventions could reduce the risk of development of disseminated stage 4 metastatic cancer later in the lifespan of the patient. Lignocaine, which is a commonly used, inexpensive, local anaesthesia drug, was thought to be one such suitable intervention because of its inhibitory effects on cancer cell division, movement and other anti-cancer properties. Depicted here is the diagrammatic representation of the technique of peri-tumoral injection which is simple and requires no additional expertise.
After completion of treatment, patients were followed up regularly for several years to compare the rates of cure and survival between the control group and the local anaesthesia group. When enough follow-up had happened in both groups the data was analysed at a cut-off date of September 2021. As expected, there was no toxicity of lignocaine in patients who received it. The 6-year disease-free survival (cure rate) was 81.7% in the control group and 86.1% in the local anaesthesia group for a 26% relative reduction in the risk of cancer relapse or death with the local anaesthesia injection, which was statistically significant. Similarly, the 6-year overall survival was 86.2% versus 89.9% in the two groups for a 29% reduction in the risk of death with the local anaesthetic injection, which was also statistically significant. Depicted below are the disease-free survival and overall survival in the two study groups over time.